By Dr Brenda Baker, BDS (Hons), MSc (Conservative Dentistry) London, Southern Cross Dental Laboratories.
Treatment planning for healthy mature patients is usually uncomplicated and does not vary much from the standard type of plans that the practitioner would normally follow. For older adults, the normal alterations in the aging mouth may require variations to the usual treatment plans proposed (McGrath, C. and Bedi, R., 1999). However, the development of treatment plans for these older adults may also be made more difficult by their deteriorating status in general health, mental acuity, oral hygiene, longevity expectations, their general function, and also budget considerations.
Background
Thirteen per cent of the population in the United States is 65 years or older (“older adults”). This can be further subdivided into young-old (65-74 years) which accounts for 7% of the cohort, the old (age 75-84) 4% and the old-old (age over 85) 2% (Vincent GK, Velkoff VA 2010). Most adults over 65 years live in the community and at any one time only 3% of this population cohort live in a “skilled nursing facility” (Werner CA. 2011).
With aging populations in many countries including Australia, the proportion of adults 65 years of age or older is slowly increasing. The proportion of people aged 65 and over has increased from 1517% from 1985-2010 and the projections suggest this will rise to 23% by 2035 (http://www.ons.gov.uk/ons/rel/mortality-ageing/ focus-on-older-people/population-ageing-in-the-united-kingdomand-europe/index.html?format=hi-vis). The Australian Bureau of Statistics has predicted that 1 in 4 Australians will be aged 65 or over by 2056 (ABS 2008). Additionally, those aged 85 or over are expected to account for 5-7% of the total Australian population, up from 1.6% in 2007. Both these predictions suggest a significant increase in the numbers of older adults likely to require dental care in the future.
Older adults with a chronic condition experienced a higher rate of tooth loss and edentulism than those without a condition (Griffin SO., et al., 2012). Increasing numbers of elderly patients still require fixed and removable complete dentures (Douglass CW. et al., 2002).
Sixty-four per cent of older adults have either moderate or severe periodontitis. Of these about 20% have both untreated coronal caries (Eke Pl., et al., 2012) and xerostomia (Turner, M.D. and Ship, J.A., 2007). Older adults continue to seek dental care and studies have shown the dental utilisation among older adults increased from 38% to 42% from 2000-2011.
Geriatric dental practice is different from providing care in traditional practice (Holm-Pedersen P., et al., 2015).Several factors differentiate geriatric dentistry from the traditional practice of dentistry:
- Older adults vary considerably and have highly variable treatment needs.
- The 65+ year-old patient is not easy to categorise. Some older Brenda Baker adults are healthy, active, financially secure individuals while others are older than their years, in poor health and live on f ixed small resources. Circumstances may also change rapidly in this age group so treatment plans require flexibility in staging and incorporate contingencies should a patient’s circumstances change.
Older adults may also be less likely to manage long treatment appointments, have transport and mobility issues, yet require multiple appointments to restore and maintain oral health. This requires careful scheduling at the practice level.
86% of this population group has at least one major chronic disorder, most commonly arthritis, osteoporosis, cardiovascular disease, cancer, neurological disorder, diabetes, mental illness or respiratory disease.
Disturbances in the oral environment may be the initial clues to systemic diseases in any patient but are of particular importance in the aging dental patient. - Polypharmacy
Polypharmacy describes the simultaneous use of numerous medications and can be a significant issue in the older population as a result of lack of compliance with drug regimens and increased risk of drug interactions (Jablonski RY., Barber MW., 2015).
More than 500 drugs in 42 categories can affect salivary flow. Gingival enlargements, altered taste and tardive dyskinesia are other known side effects of often prescribed medications (Singh, M.L. and Papas, A., 2014).
A dehydrated patient will often present with a dry mouth. Some of the major causes of dehydration include medications often used to control blood pressure and depression. Management of debilitated patients in collaboration with medical practitioners and/or pharmacists or other healthcare providers is prudent. - 20% of this group suffers from cognitive dysfunction or depression.
- The geriatric population often suffers from physical disabilities which may affect the ability of the patient to comply. This manifests itself in difficulty in maintaining adequate oral hygiene, denture hygiene or adherence to preventive regimens such as fluoride use
Access to care
The main barriers to dental care by older patients include cost, anxiety, lack of perceived need, characteristics of the dentist and availability and accessibility of dental services (Borreani E., et al., 2008).
Informed consent
Previously, the dentist/patient relationship was paternalistic and this attitude still exists amongst illiterate older adults, especially migrant groups. Patients with limited health literacy may want and need information clarified but ask fewer questions and are at greater risk of not understanding their options (Davis TC. et al., 2002). It is important to realise that the assessment of early cognitive loss is difficult and can seriously influence consent capacity (Yellowitz JA., 2005). Good communication with the older patient and their family or carer (Ettinger RL., 2015). Most older adults will give valid consent if information is communicated in a sensitive way which is mindful of the patient’s circumstances. It may be necessary to seek consent from a third party such as a legal guardian for some patients where consent is not forthcoming. Dental professionals need to allow sufficient time to obtain such consent before proceeding with invasive treatment.
Ethical Issues
All health practitioners are required to comply with the Dental Board of Australia’s Code of Conduct as a requirement of their registration.
Making decisions
Decision making is an essential part of clinical diagnosis and treatment planning which becomes more complex in functionally independent older adults as psychological problems, medication side effects, cumulative effects of traumatic disease-derived problems and iatrogenic effects on the dentition complicate dental care.
Complexity and uncertainty contribute to problems in decision making for older adults.
Uncertainty occurs when there is insufficient knowledge relative to the important variables and potential outcomes. The dentist may be uncertain about the nature of the dental problem and when or even if it should be treated, the extent of treatment based on the general health of the patient, and how much treatment the family and carers want performed.
Complexity occurs when multiple relevant variables exist. These include analysis of various treatment alternatives as well as the principles on which a decision will be based. Dental diseases are not always associated with a specific curative therapy. An example of complexity is a patient who has root caries and how the lesion is treated. The ability of the patient to maintain daily hygiene, xerostomic potential of any medications, size and activity (active or arrested) of the lesion, access to the lesion, isolation of the lesion during restoration, proximity to CEJ, margin placement, f it of the restoration to existing appliances and aesthetics are all governing factors which require consideration. Once these factors have been evaluated a suitable restorative approach can be considered:
a. Use of topical fluorides for remineralisation
b. Recontouring to reduce plaque retention
c. Use of appropriate restorative materials – glass ionomer cements/ composite resin
d. Removal of tooth/teeth and their replacement with more durable prostheses, where the prognosis of the tooth or teeth is poor.
Treatment Planning Models
Various models exist for treatment planning. The rational treatment model studies the influence of modifying factors on primary factors, which then alter the biofilm and thus the development of oral diseases and conditions (Ettinger RL., 2010). The modifying factors include lifestyle, socioeconomic status, medications, cognition, disability and medical and dental history which can alter the balance of diet, saliva and genetics, and can affect chemotherapeutics and oral hygiene. This model explains how etiologic factors affect caries development, periodontal disease, tooth loss and mucosal lesions.
Treatment plans differ in the breadth and extent of services that are needed. Risks and benefits of treatment also affect whether no treatment, emergency care, limited treatment or comprehensive care is proposed. Comprehensive treatment plans will incorporate more complex, multi-step, multi-disciplinary procedures. The patient’s desires, expectations, dental requirements, stress tolerance, financial status and ability to maintain oral health care and the experience and skill of the dentist will direct the treatment planning process (Ettinger RL., 2006).
Another geriatric assessment uses OSCAR (Shay K., 1994) which is a useful tool for dentists starting to treat older adults with complex medical problems.
O = ORAL evaluates teeth, prostheses, peridontium, pulp status, oral mucosa, occlusion, saliva.
S = SYSTEMIC evaluates normative age changes, medical diagnosis, pharmacologic agents and interdisciplinary dialogue.
C = CAPABILITY evaluates functional ability – eg. self-care, oral hygiene, caregivers, need for transport and mobility.
A = AUTONOMY evaluates ability to provide informed consent or dependence on others.
R = REALITY evaluates prioritising health care, financial limitation and life expectancy.
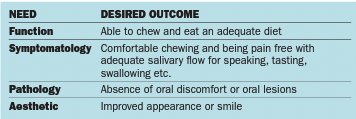
Berkey DB. et al., 1996 proposed a different conceptual model. They suggested that in clinical decision making for older adults, there were four domains of dental need that should be integrated.
The four domains of dental need:
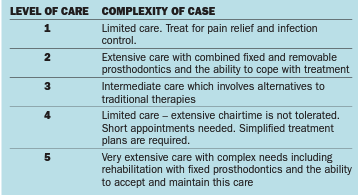
There are five levels of need to be determined to assess patient care:
Certain patient-related factors can directly affect the prognosis and complexity of dental treatment-health of the patient, neuromuscular adaptability and patient motivation. The best therapeutic option should be chosen and the clinician has to be mindful that the health status of the patient is dynamic.

